The Role of Bacteria in Mental Health Disorders
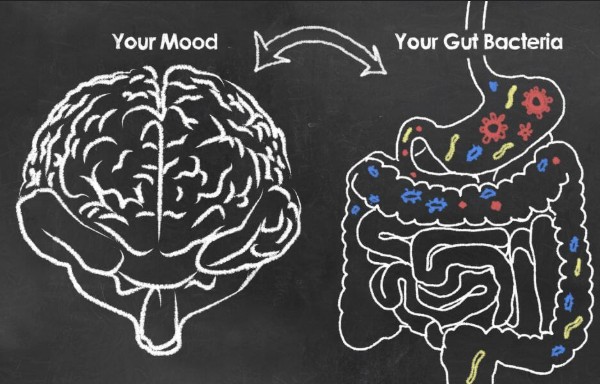
In recent years, the scientific community has developed a growing interest in the relationship between the gut microbiota and mental health. This emerging field of research, often referred to as the “gut-brain axis,” explores how the bacteria residing in our intestines might influence mental health disorders. This discovery has the potential to revolutionize our understanding of psychological disorders and pave the way for innovative treatment methods.
The Gut-Brain Connection
The gut-brain axis refers to the complex communication network that links the intestines and the brain. It involves multiple pathways, including neural, hormonal, and immunological signals. Research has shown that the gut microbiota can produce neurotransmitters like serotonin and dopamine, which play critical roles in mood regulation.
How Bacteria Communicate with the Brain
Understanding how bacteria in the gut communicate with the brain is essential. This communication occurs through several mechanisms:
- Vagal Nerve Stimulation: The vagus nerve acts as a highway between the gut and the brain, transmitting information about the body’s state, including microbial composition.
- Neurotransmitter Production: Gut bacteria can produce and modulate the levels of neurotransmitters that impact brain function.
- Immune System Modulation: The gut microbiota interacts with the immune system, influencing inflammation—a factor linked to various mental health disorders.
Impact of Gut Microbiota on Mental Health Disorders
Emerging studies have established a correlation between gut health and mental well-being. Here are some notable mental health disorders that may be influenced by gut bacteria:
Anxiety and Depression
The link between gut health and mood disorders like anxiety and depression is a hot topic in research. Studies suggest that individuals with depression often have an imbalance in their gut microbiota. Treatments aimed at restoring this balance, such as probiotics, have shown promise in alleviating symptoms.
- Probiotics as a Treatment: Probiotic supplements, often termed “psychobiotics,” have been found to reduce anxiety and depressive symptoms in human and animal studies.
- Dietary Interventions: Diets rich in fiber and fermented foods support a healthy gut microbiome, potentially reducing anxiety and depression risks.
Autism Spectrum Disorder (ASD)
Research into the role of gut bacteria in autism spectrum disorders suggests that individuals with ASD often have distinct gut microbiota profiles compared to neurotypical individuals. Altering these microbial populations through diet or probiotics may influence behavioral symptoms.
- Microbiome Transplant: Fecal microbiota transplantation has shown initial success in modifying symptoms of ASD.
- Dietary Modifications: Implementing specific diets that promote beneficial bacteria might improve ASD symptoms.
Schizophrenia
Although in its early stages, research has also linked gut microbiota imbalances to schizophrenia. Studies are exploring how alterations in microbial populations can exacerbate or mitigate the symptoms of this complex disorder.
- Potential Therapeutic Approaches: Targeting gut bacteria as a complementary treatment for schizophrenia is an area ripe for exploration.
The Future of Mental Health Treatments
As our understanding of the gut-brain axis advances, the potential for new treatment strategies for mental health disorders expands. The idea of targeting the gut microbiota for mental health interventions is both exciting and complex.
Personalizing Treatment
The concept of personalized medicine in mental health is becoming more tangible. By analyzing an individual’s gut microbiome, practitioners could tailor treatments to target specific microbial imbalances, leading to improved outcomes.
Challenges and Considerations
While the promise of gut microbiota-based interventions is significant, several challenges must be addressed:
- Individual Variability: Each person’s microbiome is unique, which could result in variable responses to treatments.
- Ethical and Safety Concerns: Manipulating gut bacteria raises ethical questions and potential safety issues that require careful consideration.
- Long-term Effects: Understanding the long-term consequences of altering the gut microbiota is crucial for safe and effective interventions.
In summary, the role of bacteria in mental health disorders represents a promising frontier in science. While challenges remain, the gut-brain axis offers a new perspective on treating mental health conditions. As research continues to unravel the complexities of this relationship, the potential for groundbreaking advancements in mental health care becomes increasingly plausible.